The CHOC Health Alliance Claims Customer Service Department is here to help you with any claims inquiries, including questions about initial claims, resubmissions, and denials. We can be reached at 800-387-1103.
Claim forms
To get started on filing a claim, click the appropriate form below and follow the instructions:
CMS 1500 Form
CMS UB-04 Form
When completing the claim form, please remember:
- Claims must be legible and suitable for imaging and/or microfilming for permanent record retention.
- Complete all required fields and include additional documentation for medical necessity, such as medical records.
- Claim form may be returned unprocessed (Void) if illegible, poor quality copies are submitted, or required documentation is missing. This could also result in the claim being denied.
Submit claims electronically
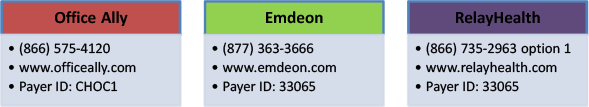
Submitting claims electronically is safe, faster, and easier to track than paper claims. If you are not already using an electronic billing system, you may contact a clearinghouse directly, at the following:

Encounters must be submitted for all services provided to CHOC Health Alliance (CHA) Members, whether the services are capitated or fee-for-service. This includes all CHDP visits (full & partial assessments, immunizations, and sick visits). We strongly encourage electronic claim and encounter submission as it provides your office with benefits including: ensuring HIPAA compliance, increasing accuracy of data, and reducing operational costs associated with paper claims.
To facilitate your electronic submission, claims and encounters can be submitted to CHOC Health Alliance through any of the following clearinghouses:
If electronic submission is not an option, all claims and encounters can be mailed to Rady Children’s Hospital, Attn: CHOC/CPN Claims 3020 Children’s Way, Mail Code 5144, San Diego, CA 92123.
Submission of claims and encounters is a contractual requirement, and electronic submission is being monitored as part of CHA’s 2016 Quality Metrics Incentive Program. For questions about this memo, please contact your Provider Relations Representative.
We look forward to working collaboratively with you and your office staff, and appreciate the quality care you provide to our members.
Standards for Electronic Transactions – New Versions, New Standard and New Code Set – Final Rules:
Regulations and guidance to transaction & code sets standards can be found by visiting the website, Transaction & Code Sets Standards.
Submitting paper claims
If you cannot submit claims electronically, please mail paper claims to the address below. Remember to include supporting medical documentation when necessary.
Rady Children’s Hospital San Diego
CHOC/CPN Claims
3020 Children’s Way, Mail Code 5144
San Diego CA 92123
Claim resubmissions or reconsideration
DEFINITIONS:
Resubmission– is defined as a claim originally denied because of missing documentation, incorrect coding etc., for which you are now submitting the required documentation and resubmitting a request for payment.
Reconsideration– is defined as a request for review of a claim that you believe was incorrectly paid or denied because of a processing error.
When filing a claim resubmission or reconsideration , please remember to:
- Include the resubmission form, along with a brief description of the requested correction or expected outcome,
- Clearly label “Resubmission” on the claim in black ink,
- Include additional documentation if required (e.g., medical records, EOB),
- Mail your claim (s) (do not submit EDI for resubmission) to, Attn: Claims Resubmissions
How to verify claim receipt, status, or payment
To track your claim with dates of services on or before January 31, 2014, you can visit the secure web portal AboveHealth, to check the status of claims, and prior authorizations . The web portal will only be available for historical information through June 30, 2014. You can also contact Claims Customer Service Department at: (800)387-1103.
Claims with Dates of Service ON OR AFTER February 1, 2014:
- Utilize the New Secured Provider Web Portal “EZNet”
- Or you can phone Claims Customer Service at: (800) 387-1103
For additional information, review the Claims chapter of your Provider Manual.
Billing resources:
Training Seminars/webinars/eLearning tutorials
Medi-Cal offers basic, advanced seminars, and online classes for providers regarding billing.
To see a class schedule and register, visit the Medi-Cal Learning Portal (MLP).
HIPAA 5010 transaction set upgrade
HIPAA 5010 became effective January 1, 2012. Health Care Providers, health plans, and health care clearinghouses must comply with the changes to transaction set standards. The Electronic Data Interchange (EDI) HIPAA 5010 (ASC X12 5010) transaction set will help facilitate a nationwide conversion to an electronic health care environment, for more information click here.
NPI online submission
The Health Insurance Portability and Accountability Act of 1996 (HIPAA) mandated that the Secretary of Health and Human Services adopt a standard unique health identifier for Health Care Providers. As a result, all health care providers who are HIPAA-covered entities must obtain a National Provider Identifier (NPI) to identify themselves in standard electronic transactions by May 23, 2007.
These transactions include claims, eligibility inquiries and responses, claim status inquiries and responses, referrals and remittance advices.
For more information about the NPI, please visit the Centers for Medicare & Medicaid Services (CMS) website. If you have yet to obtain your NPI, you can go to the National Plan and Provider Enumeration System website or call the NPI Enumerator Call Center at 1-800-465-3203.

